The Covid-19 Testing Laboratory Guide: Covid – 19 Occurrence in Breast Cancer Patients
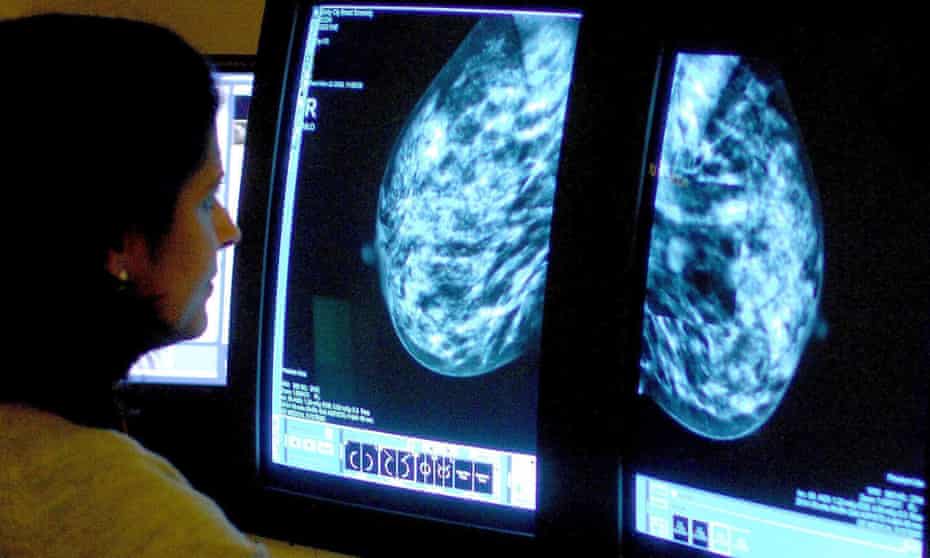
COVID-19 plays a more dangerous role in cancer patients. In the pandemic, the screening tests for breast took a sharp decline due to a shift of focus towards Covid-19 testing at Covid-19 Testing laboratory.
Background
The World Health Organization was notified on December 31, 2019, of instances of pneumonia with an unknown origin in Wuhan, China. The cause of coronavirus sickness in 2019 identification happens as a novel coronavirus known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (COVID-19).
The spread of viral outbreaks from China to the rest of the world took place during the next few months. And the WHO declared it as a pandemic. The number of confirmed cases in France grew in early March. With over 2800 cases officially recorded on March 13, 2020. Thereby, the French hospital emergency responses plan. It coordinates all hospitals. And then its upgrade happens at its maximum readiness level.
On February 14 publication of the first study on COVID-19 outcome in cancer patients happened. Out of 18 Chinese patients with a history of cancer and a diagnosis of COVID-19, 7 (39%) required intensive care unit (ICU) treatment and/or died. The findings of this key retrospective investigation raised serious concerns about COVID-19 infection in cancer patients. Further research found that cancer patients have a higher incidence of severe COVID19 symptoms and death than the overall Chinese population.
Patients with blood, lung or metastatic malignancies have the highest rate of poor outcomes, according to reports. According to a preliminary report on New Yorkers admitted to ICU. The retrospective reports are of limited size and limited to patients treated in Chinese hospitals. However, they may not be entirely transposable to Western healthcare systems.
COVID-19 Diagnosis In Cancer Patients
Testing at Covid-19 Testing laboratory initially faced limitations to severely sick patients with COVID-19 symptoms. But by the end of March 2020, it was open to all cancer patients with suspected COVID-19 (even outpatients receiving active therapy).
Reverse transcription-polymerase chain reaction assays target two areas of the viral RdRp gene. Its utilization occurs in looking for SARS-CoV-2 RNA in swabs. The French National Reference Center had to validate all tests used in France (Institut Pasteur, Paris, France)
What Breast Cancer Patients Should Know
The respiratory infection known as “coronavirus” and officially known as COVID-19 has altered our way of life. According to the Centers for Disease Control and Prevention (CDC), most persons have a minimal chance of being critically ill with COVID-19. It’s crucial to note, however, that persons who have been diagnosed with cancer, including breast cancer, are at a higher risk of developing serious sickness if they get COVID-19. A history of cancer may also raise your chances of getting sick with COVID-19. Later getting a diagnosis at Covid-19 Testing laboratory.
Chemotherapy, targeted therapies, and immunotherapy are some of the breast cancer treatments that can weaken the immune system and create lung difficulties. If infected with the coronavirus, people with compromised immune systems or lung difficulties are at a considerably higher risk of serious repercussions.
After completing these breast cancer therapies, most people’s immune systems recover within a few months. However, the time it takes for your immune system to heal varies and is dependent on a number of factors. It’s unclear whether you’re at a larger risk of major COVID-19 problems if you’ve had these therapies before.
People who have breast cancer that has progressed to the lungs may develop COVID-19, which can make their lung difficulties worse.
It’s critical to follow the CDC’s recommendations for wearing a mask and physically separating yourself from others. As well as get vaccinated anytime. And if you can stay at home. Protect yourself and help reduce the spread of the virus. During the COVID-19 pandemic, if you or a loved one gets treatment for breast cancer. Don’t panic, simply follow the above guidelines.
Impact of Covid – 19 on Immunity
COVID-19 (severe coronavirus illness) leads immune cells to become hyperactive, resulting in lung inflammation. COVID-19 induces the production of factors previously linked to the reawakening of dormant breast cancer cells, such as neutrophil extracellular traps, according to recent research (NETs). As a result, the presence of NETs and a pro-inflammatory milieu may encourage breast cancer reactivation, thereby raising the likelihood of pulmonary metastasis.
More research is needed at Covid-19 Testing laboratory. For the confirmation of the association between COVID-19 and cancer recurrence. Increased understanding of COVID-19’s potential hazards for breast cancer patients could lead to better treatment techniques to prevent metastatic relapse.
Is It Safe To Postpone or Adjust Breast Cancer Screening or Treatment?
Elective procedures include screenings, surgeries, and other treatments. The delaying and cancellation of some procedures happened. Because they were not considered urgent, emergencies. Or otherwise needed for life-threatening disorders. Many hospitals and other healthcare facilities at the start of the epidemic did that. It was upsetting whether it happened to you or a loved one. If you were scheduled for a cancer test, surgery, or other treatment, you undoubtedly felt compelled to go.
However, these difficult decisions helped in safeguarding people from contracting COVID-19 while in a healthcare facility. And to ensure that healthcare providers had the tools. They needed to treat patients with severe COVID-19 infections. And early diagnosis at Covid-19 Testing laboratory plays a pivotal role.
Is It Possible To Acquire A COVID-19 Vaccine If You Have Breast Cancer?
Yes, in most situations, the three COVID-19 vaccines available in the United States are deemed safe and effective for persons who are getting cancer therapy or have a history of cancer. People receiving cancer therapy should be vaccinated, according to the CDC, the National Comprehensive Cancer Network (NCCN), and other expert medical organizations. Still, because everyone’s condition is unique, you should see your doctor about becoming vaccinated, as well as if and how many boosters you should have if you are already completely vaccinated.






